Report on Mission to help develop adult and adult congenital heart surgery at the Jakaya Kikwete Cardiac Institute Dar es Salaam, Tanzania.
January 12th – 24th, 2020
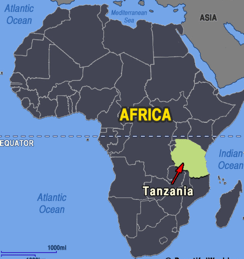 CardioStart’s third mission to The Jakaya Kikwete Cardiac Institute (JKCI) in Dar es Salaam took place January of this year. The Republic of Tanzania was formed as a sovereign state in 1964 through the union of the separate states of Tanganyika and Zanzibar. Mainland Tanganyika covers more than 99 percent of the combined territories’ total area. It is bound by 7 countries through its borders and is South of the Equator. Dodoma, since 1974 the designated official capital of Tanzania, is centrally located on the mainland. Dar es Salaam, (in Arabic, meaning ‘Haven of Peace’ remains the seat of most government administration, as well as being the largest city and port in the country. It has Africa’s highest mountain, Kilimanjaro (19,340 feet), and the world’s second deepest lake, Lake Tanganyika (4,710 feet deep). The majority of Tanzanians are of Bantu descent. A third of the population is Christians and slightly more are Muslim. The two principal languages are Swahili and English. The economy is largely agrarian.
CardioStart’s third mission to The Jakaya Kikwete Cardiac Institute (JKCI) in Dar es Salaam took place January of this year. The Republic of Tanzania was formed as a sovereign state in 1964 through the union of the separate states of Tanganyika and Zanzibar. Mainland Tanganyika covers more than 99 percent of the combined territories’ total area. It is bound by 7 countries through its borders and is South of the Equator. Dodoma, since 1974 the designated official capital of Tanzania, is centrally located on the mainland. Dar es Salaam, (in Arabic, meaning ‘Haven of Peace’ remains the seat of most government administration, as well as being the largest city and port in the country. It has Africa’s highest mountain, Kilimanjaro (19,340 feet), and the world’s second deepest lake, Lake Tanganyika (4,710 feet deep). The majority of Tanzanians are of Bantu descent. A third of the population is Christians and slightly more are Muslim. The two principal languages are Swahili and English. The economy is largely agrarian.
Cardiac Surgery Status in Dar es Salaam
JKCI continues to be the only cardiac institute in the country and to attract patients from some surrounding countries. It is affiliated with the University, with junior doctors rotating through the specialties there; local team leaders strongly emphasize and value teaching models. The hospital has 128 beds, including 15 ICU beds (combined pediatric and adult), 3 OR theaters (still, only 2 are being used). JKCI also has an adult cardiac ward for pre and post-operative adult patients and a new pediatric ward and ICU in the adjacent children’s hospital building. There are not yet any cardiac operating theatres in the children’s hospital building. Currently, during the initial post-operative period, pediatric patients are cared for in the combined adult and pediatric ICU at JKCI. Once felt to be stable, they are moved to the pediatric ICU and ultimately, the pediatric ward in the children’s hospital building.
It should be noted that JKCI is not only a surgical center but strives to provide comprehensive care to cardiac patients; they have a busy cardiac catheter laboratory and an outpatient clinic (open 6 days a week). The institute is funded publicly. The need for ongoing cardiac surgery development is dire as is developing a comprehensive adult peri-operative ICU program and developing further the pediatric peri-operative ICU program in order to ensure success and sustainability of the cardiac surgical programs.
Although the local cardiac surgeons are taking on some more complex surgical cases independently (especially, the pediatric cardiac surgeons), most complex, high risk cases are generally sent to India. As with other countries in Africa, there are very few centers doing cardiac surgery and even then, many are functioning at the minimal volume level. One of several factors that limits the number of cardiac surgical cases that can be done locally is not having a resource for or access to bio-prosthetic heart valves. JKCI leadership continue to seek resources that will contribute to continued growth, evolution and sustainability of their programs; which will require expansion of existing facilities or adding new facilities and equipment, hiring more staff; and providing ongoing and additional training for current staff.
OUR MISSION FOCUS:
- ADULT AND PEDIATRICS CARDIAC SURGERY – BOTH CONGENITAL AND ACQUIRED CASES
- PROVIDE SUPPORT & GUIDANCE TO THE LOCAL TEAM (SURGEONS, ANESTHESIOLOGISTS, INTENSIVISTS, PERFUSIONISTS AND NURSES)
Mission building objectives: these were met by the following actions:
 1. OR
1. OR
Surgery:
All cases were carried out with the local team performing cases as the primary surgeons and the operating list illustrates the wide-ranging complexity of the cases carried out. Planning and execution of the preparatory (pre—bypass components of surgical procedures were extensively discussed. Intra-operative teaching was carried out in valve repair/replacement techniques, multi-valve presentations, strategies for myocardial protection and de-airing, and coronary bypass grafting). Assistance and guidance were also given to the local pediatric cardiac surgeons with more complex congenital cardiac cases.
Anesthesia:
Mentoring was provided chiefly in the adult cases undertaken, and the CardioStart anesthesia expert taught advanced techniques in peri-operative clinical management and intra-operative echocardiography. Pediatric anesthesia was felt by the CardioStart pediatric cardiac surgeon to be managed very well by the local team.
Perfusion:
Support was given by the CardioStart perfusionists to the local perfusion team in both pediatric and adult cases. The CardioStart perfusionists have provided very constructive feedback and suggestions with regard to equipment and perfusion regimens to feedback to the local team.
OR Advanced Teaching:
Emphasis on algorithms and procedural issues were provided in the OR and support given during the complex cases. Explanted valve tissue was collected and held by the CardioStart OR nurse, for an ongoing study of tissue harvested during certain cases in collaboration with Local Tanzanian cardiologist, Dr. Khuzeima Khanbhai, and the University of Minnesota (Dr. Bryce Binstadt).
 2. Cardiac ICU:
2. Cardiac ICU:
Clinical:
JKCI’s local pediatric intensivist has put forth tremendous effort towards teaching the JKCI ICU nursing staff with respect to medical management and in developing a culture of safety. During the mission, the CardioStart multidisciplinary team along with the local team conducted bedside teaching pertinent to the patients. The surgical case mix was such that most patients did very well, with routine post-operative medical courses. There were, however, a few patients that proved to be particularly challenging; providing many opportunities for the CardioStart nurses to point out, explain and demonstrate the vital role that cardiac ICU nurses play in the stabilization and ongoing management of post-operative cardiac patients.
Advanced Teaching:
CardioStart nurses provided additional guidance and instruction, support by from the CardioStart intensivist/cardiologist when they identified areas in which the local nursing staff would benefit from additional training essential to meet recommended standards. Based on input and collaborative discussion with the CardioStart nurses and intensivist, the JKCI ICU team made adjustments to the data form they use for reporting on morning rounds. Also stressed during this mission was the importance of consistently conducting formal, structured patient handovers when transitioning care of the patient from the OR to the ICU; (a strategy is the practice that has been the subject of many studies and publications concerning error and patient safety). The JKCI team see this as a work in progress and plan to review as they go, making any changes they think will improve the consistency and continuity of patient care.
Adult Patients who underwent surgery
|
Name |
Operation |
Outcome |
|
C.B., 65y |
3-vessel CABG |
Satisfactory |
|
H.T., 42y |
MV replacement w/mechanical valve |
Satisfactory |
|
B.S., 56y |
ASD repair |
Satisfactory |
|
M.J.M., 53y |
MV replacement |
Satisfactory |
|
J.S., 18y |
MV replacement |
Satisfactory |
|
H.H., 34y |
MV replacement w/mechanical valve, TV annuloplasty (redo) |
Satisfactory |
|
N.M., 37y |
AoV, MV both replaced w/ mech. valve, TV annuloplasty ring |
Died of MSOF* |
|
S.A., 59y |
3-Vessel CABG |
Satisfactory |
|
R.N., 19y |
MV Replacement (redo) |
Satisfactory |
|
* Known very high risk; patient deemed to need, and was offered surgery 4 years previously but refused. He requested surgery once he had developed end stage heart failure. He and his family understood the risk and chose to proceed. |
||
Pediatric Patients who Underwent Surgery
|
Name |
Diagnosis/Operation |
Outcome |
|
H.S.S., 11y |
Double Chamber RV(DCRV), VSD/DCRV Resection, VSD closure |
Satisfactory |
|
F.N.L., 6y |
ASD /ASD repair |
Satisfactory |
|
E.J.G., 8y |
Doubly chamber RV, VSD, PDA/ DCRV Resection, VSD closure, PDA ligation |
Satisfactory |
|
H.M.S., 15y |
Rheumatic Heart Disease /MV replacement, chordae repair |
Satisfactory |
|
I.K.D., 3y |
Tricuspid atresia/ BCPS*, Brisbane Procedure |
Satisfactory |
|
F.S.G., 8y |
TOF Repair |
Satisfactory |
|
J.S., 15y |
Rheumatic, severe MR, Pulm HTN/MV Repair, annuloplasty |
Satisfactory |
|
R.M., 10y |
VSD Closure |
Satisfactory |
|
R.M.N., 12y |
BCPS, Brisbane Procedure |
Satisfactory |
|
A.A.M., 20mos |
Partial AVSD/ AVSD repair |
Satisfactory |
|
J.L.M., 2y 9mos |
VSD closure, PDA ligation, |
Satisfactory |
|
P.R.T., 4ys |
Closure of AP window, subaortic membrane resection |
Satisfactory |
|
I.J.H., 5mos |
Truncus arteriosus, Type 2, proximal RPA stenosis/Truncus repair |
Satisfactory |
|
B.A.S., 2y |
Ao arch reconstruction, PDA division, SubAo membrane resection |
Satisfactory ** |
|
J.J.T., 6mos |
DORV w/large VSD/ PA band |
Satisfactory |
|
F.A.A., 1y |
Doubly committed restrictive VSD (L-to-R) , mod MR, mild-mod AR/ VSD Closure |
Satisfactory |
|
* Bidirectional Cavopulmonary Shunt (also referred to as Bidirectional Glenn) |
||
|
** Did well initially but had a cardio-respiratory arrest on the afternoon of POD #1; (2° to ventilator malfunction). He was successfully resuscitated with satisfactory outcome. |
||
 3. Additional Education; Cardio-pulmonary Resuscitation:
3. Additional Education; Cardio-pulmonary Resuscitation:
Several CardioStart volunteers conducted a comprehensive combined resuscitation and peri-operative care course over 3 days which was well attended and received by nurses, physicians (staff and trainees) and medical students. It included many principals from Basic Life Support (BLS), Pediatric Advanced Life Support (PALS) and Advanced Cardiac Life Support (ACLS) in addition to lectures pertaining to pre-operative, intra-operative and post-operative care. Teaching involved use of mannikins, visual guides, computer aided programs and intubation equipment brought in from California. Various clinical presentations and appropriate resuscitative techniques were fully covered within lectures and practical stations. Each local team member was encouraged to practice these techniques on the mannikins with course instructors present to observe, answer questions and when needed to help and provide feedback.
 Acknowledgements:
Acknowledgements:
We acknowledge with gratitude a number of individuals and corporations who facilitated this mission.
- Prof. Mohamed Janabi, CEO, and colleagues at JKCI
- Accuware Consultants Inc., Ohio, USA medical equipment donations
- Amy Lauth Foundation, Virginia, USA (funding & freight logistics)
- CardioStart Administration Team, Tampa, Florida, USA (logistics)
- CardioStart ReSale Thrift, Oregon, USA (Database and general funding support)
- Edward LifeSciences Inc. (CA, USA) for bio prosthetic valves (through Americares Inc)
- Americares, (CT, USA), for valves, medication and Life-box pulse-oximetry donations.
- SonoSite, for loaning us an ultrasound machine through their Global Loner Program
- Southtowne Rotary Club, (Eugene, OR, USA) for equipment donations & Logistics
- Dr. Farah Rahman, (PA,USA). (Donation of surgical hand-sewn hats and blankets)
- United Methodist Church, Lake Oswego, OR, USA) (Children’s doll gifts)
- California Medical Training Center, (CA, USA) for mannikin aids in CPR and resuscitation training
- Donations carried in suitcases by individual CardioStart team members
 CardioStart Team:
CardioStart Team:
- Mission Director: Pediatric Cardiac Intensivist: Dr. Barbara Ferdman (USA)
- Mission Coordinator and Respiratory Therapist: Lynn Leslie, (USA)
- Surgeons: Dr. Tom Karl (USA), Dr. Donato Sisto (USA), Dr. Bill Wilson (USA), Dr. Aubyn Marath (USA).
- Adult Anaesthetist: Dr. Michael Schupp (UK).
- Perfusionists: Neil Casey (CA), Bill Nicotra (USA)
- Adult Cardiac ICU Nurse: Stacy Adams (USA)
- Pediatric Cardiac ICU Nurses: Rachal Dorvall (USA), Griffin Marube Anasi (Kenya)
- OR Nurse: Leslie Morse (USA)
- Database Collators: Liz Marut (USA), Rosalie Keta Mbumba (Democratic Republic of Congo)
- Team Assist: Isobel Casey (CA)
- Resuscitation Course Coordinators, Lead Instructors: Michael Pyorala, Dr. Rich Harper
Team social activity
Most of the CardioStart team had traveled very long distances across continents to join the mission and participate; the group were also supported by other African countries helping the Tanzanians: one member came from Kenya (pediatric ICU nursing) and another, from Democratic Republic of the Congo (Database collation). During the middle weekend, team members took a short trip to the island Zanzibar. It has soft sandy beaches, a strong Arabic influence, a collection of spice farms and a World Heritage Site, the historic city of Stonetown, which was grimly associated with a flourishing slave trade, more than two centuries ago. At the end of the mission, several volunteers finished their assignment exploring the region.
 Reflections:
Reflections:
In the 6-month interval between the CardioStart mission in July 2019 and January 2020 there has been a noticeable increase in the complexity and number of pediatric and adult surgical cases. Going forward in addition to providing guidance and support from a surgical standpoint, it will be equally if not more important to provide additional and ongoing support and guidance with respect to ICU nursing, perfusion and cardiac anesthesia (particularly in the adult OR). Based on this and the previous CardioStart missions to JKCI it became very clear that the presence or absence of an RT from the CardioStart team had a significant impact on patient care and outcomes. Currently, there are no RT’s in Tanzania. So, having an opportunity to work with and learn from the CardioStart RT was beneficial not only to patient care but also helped to raise awareness of the JKCI team and administration to the value and importance of having RT’s on their team. Overall, the program is evolving and with plans that will allow for continued growth and development of the Institute towards becoming a sustainable, autonomous entity, a model for other countries of similar size and at a similar stage of development.
 Post-Mission Objectives:
Post-Mission Objectives:
- CardioStart anesthesia volunteer, Dr. Schupp, plans to bring back one of the JKCI VividQ ultrasound/echocardiography machines for repair in the UK and JKCI will need to arrange transport back to Dar Es Salaam. He has also provided JKCI with recommendations pertaining to the anesthetic machines, syringe pumps and maintenance of all equipment to ensure they are in working order and up to accepted safety standards
- JKCI had agreed to have an intra-aortic balloon pump on hand for this mission but were unable to get one. CardioStart has encouraged JKCI administration to purchase or obtain one prior to operating on very high-risk adult patients likely to require post-operative mechanical support.
- JKCI and CardioStart intensivists are planning ongoing collaboration with the clinical curriculum development and research projects that will provide insight into their program, contribute to the body of literature already existing and other projects in which CardioStart volunteers are engaged.
Leave A Comment